The world of weight loss medications is being reevaluated following a study led by Professor Donal O'Shea of St. Vincent's University Hospital (SVUH) and the UCD School of Medicine. The research focused on the medication Ozempic, a drug that has been under public scrutiny for some time. The study's findings, published in the Journal of the Obesity Society, challenge the prevailing belief that weight loss medications like Ozempic, Wegovy, or Monjaro primarily work by promoting satiety and reducing food intake.
The research involved a randomised controlled trial with 30 patients and focused on medications based on the hormone Glucagon-like peptide-1 (GLP-1). The findings reveal a strong relationship between increased metabolic activity caused by daily GLP-1 treatment and the amount of weight lost. Interestingly, individuals with lower metabolic activity before beginning treatment experienced the most significant benefits.
This study challenges the main narrative about these newer treatments, which is that they simply make you eat less and that any action on energy burn is minimal, said O'Shea. The strength of the association is surprising given the relatively small number of participants, suggesting that this increase in metabolic activity is a significant contributor to how these drugs work.
O'Shea emphasised the importance of understanding the full mechanism behind these treatments. Safe medical treatment for obesity is still in its infancy, and we need to fully understand how the treatment works. Understanding how these agents increase energy burn should be an important part of future research.

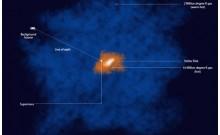
The study was co-authored by Professor Silke Ryan, SVUH, funded by the Health Research Board and supported by University College Dublin. The 30 subjects had specialised imaging of the fat within their abdomen using a PET-CT scanner, with scans carried out before and after six months of treatment.
The findings of this study are significant as they challenge the existing understanding of how these weight loss medications work. It reveals that these drugs do not just suppress appetite but also significantly increase metabolic activity, contributing to weight loss. This is especially true for individuals with lower metabolic activity before treatment.
This study also highlights the need for a more comprehensive understanding of these treatments. As O'Shea points out, safe medical treatment for obesity is still in its infancy, and there is a need to fully understand how these treatments work. This includes understanding how these agents increase energy burn, which should be an important part of future research.
The findings of this study also shed light on the uncomfortable truth about the diet industry. The industry has been long criticised for its inhumanity and the unrealistic standards it promotes, especially among people in the public eye such as actors and models. Some of these individuals have been candid about their struggles to maintain the size zero figure. This study brings to the fore the need for a more humane and realistic approach to weight loss and body image.