A new implantes sensor system created by researchers from MIT can be used to track tumours or even dispense drugs inside the bodies of patients. The idea is to make exploratory studies in patients without surgery or having them swallow tubes with embedded cameras.
This in-body GPS system, say its makers will be less expensive, invasive and time-consuming. To this end, a team of researchers from MIT's Computer Science and Artificial Intelligence Laboratory (CSAIL) are working on "ReMix".
In a statement put out by the research team, they say that ReMix can actually pinpoint the exact location of ingestible implants inside the body. It makes use of using low-power wireless signals for this. When tests were run on animals, the team demonstrated that it is possible, using ReMix to track implants inside the animal down to a centimetre. They added that as the tech on it gets better, over time, similar implants might be used to deliver drugs to specific parts of the body.
Dina Katabi of MIT led this study. She previously developed a method to use wireless signals and detect movement and vital signs as subtle as the rise and fall of a baby's chest from an adjacent room.
Implanting Marker
To test the ReMix, Katabi's group reportedly first implanted a small marker in animal's tissue. Then, to track its movements, a wireless device that reflects radio signals off the patient, and an AI was used to pinpoint the exact location of the marker. Researchers explained that signals need not actually be generated by the marker inside the patient's body, rather, it simply reflects incoming signals transmitted by ReMix from outside the body.
One of the key challenges in having wireless signals work this way is the numerous other reflections that tend bounce off a human body and cloud up the signals. In fact, say the researchers, signals that reflect off the skin can be up to 100 million times stronger than signals reflected off the embedded marker itself.
To overcome this, the team had to come up with a way to essentially separate interfering skin signals from ones they are looking for. Using a small diode that can mix signals together, the team was able to then filter out the skin-related signals.
How it works?
As to how it was done, if the skin reflects frequencies of F1 and F2, for example, the diode then creates new combinations of those frequencies such as F1-F2 and F1+F2. The system then waits for the signals to get reflected back and only picks up combined frequencies this filters out all the signals that bounced off the patient's skin.
"The ability to continuously sense inside the human body has largely been a distant dream," says Romit Roy Choudhury, a professor of electrical engineering and computer science at the University of Illinois, who was not involved in the research.
One of the roadblocks, he says, has been wireless communication to a device and its continuous localization. ReMix makes a leap in this direction by showing how the wireless component of implantable devices no longer need be this bottleneck.
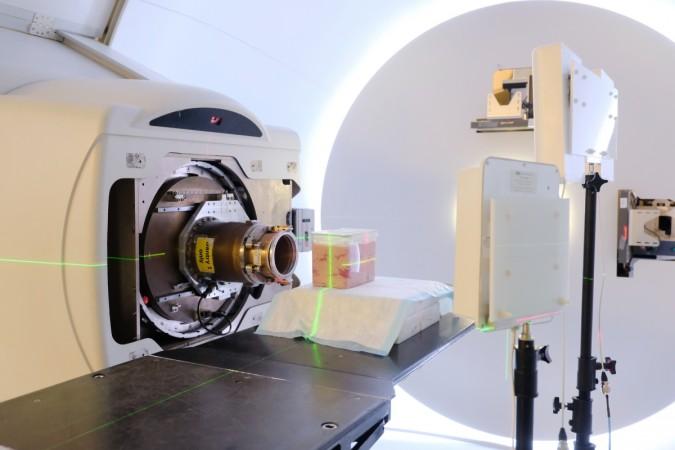
Proton Therapy
One of the potential applications for ReMix, says the statement, is proton therapy. It is a type of cancer treatment that has magnet-controlled protons fired directly at tumours till they wither away. Treatment is targeted specifically at erring tumours so it makes it possible for doctors to prescribe high doses of radiation, and because of the level of radiation involved, the procedure naturally requires a high degree of precision, this is why proton therapy is usually limited to only certain types of cancers.
The success of this therapy hinges on the target tumour staying put and not moving at all during the radiation process. If said tumor moves, then healthy tissue could be exposed to radiation. However, with just a small marker, doctors could then better locate the tumour in real-time and make sure the radiation reaches only the affected tissue.
As of now, ReMix is still under development and not yet accurate enough to be used in clinical settings, says Katabi. A margin of error closer to a couple of millimetres would be necessary for actual implementation, she added.