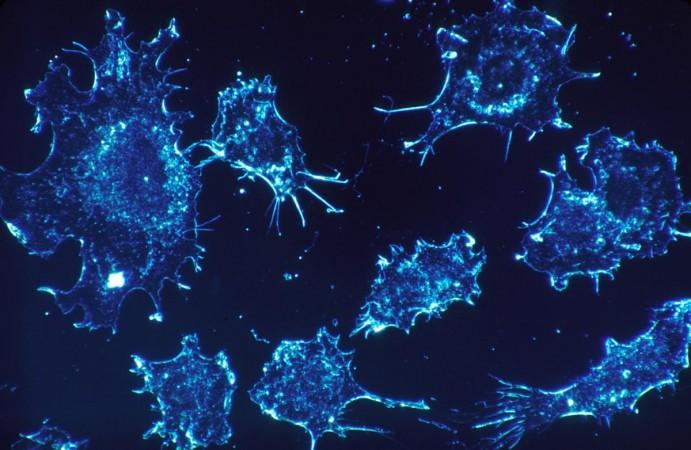
There is no silver lining when it comes to the form of cancer one is struck with. However, localized cancers make treatment relatively easier. However, metastatic cancers—that begin in one part of the body and spread to others—are complexly difficult to treat. Lungs are the most common targets of metastasis, which results in the formation of tumors. Now, scientists have developed a treatment using a plant virus that may prevent metastasis within the lungs.
In a new study, researchers from the University of California San Diego have described the development of a new treatment utilizing nanoparticles derived from cowpea mosaic virus (CPMV), a plant pathogen. Using an animal model, the authors demonstrated that the treatment slowed the growth of tumors in the lungs of subjects with either metastatic breast cancer or melanoma.
The team also showed that nanoparticles prevented or significantly reduced the spread of the two cancers to the lungs of healthy animals when they were challenged with them. "Because these nanoparticles tend to localize in the lungs, they can change the tumor microenvironment there to become more adept at fighting off cancer — not just established tumors, but future tumors as well," said Eric Chung, co-first author of the study, in a statement. The findings were published in the journal Advanced Science.
Turning to a Plant Virus

Plant viruses cannot cause infection in the human body. However, they register as a foreign invader or substance. This can trigger danger signals that cause immune cells to enter attack mode and seek out a pathogen. The authors aimed to leverage this property of plant viruses to help the immune system identify cancer cells and destroy them, particularly lung tumors that arise as a result of metastatic cancers.
The authors hade demonstrated in previous studies that cowpea mosaic virus acts as an adjuvant when administered intratumorally (directly into the tumor). They had learnt that this approach led to the recruitment and activation of innate immune cells in the lungs. This was followed by tumor cell killing (mediated by natural killer cells and neutrophils) and tumor antigen processing. Ultimately the adaptive arm of the immune system was activated, which resulted in cell-mediated systemic anti-tumor immunity.
Deriving Plant Virus Nanoparticles
In order to utilize this immune response to lung tumors, the team engineered nanoparticles synthesized from the cowpea mosaic virus to seek out a protein called S100A9 in the lungs. For the development of the nanoparticles, black-eyed pea plants were grown in the lab and infected with the virus. The virus was harvested in the form of ball-shaped nanoparticles. Following this, S100A9-targeting molecules were attached to the surface of the obtained nanoparticles.

Immune cells that aid in fighting infections within the lungs, express and secrete S100A9. However, a crucial factor led the researchers to choose S100A9 as a target: overexpression of this protein has been found to play a role in the growth and spread of tumors.
"For our immunotherapy to work in the setting of lung metastasis, we need to target our nanoparticles to the lung. Therefore, we created these plant virus nanoparticles to home in on the lungs by making use of S100A9 as the target protein. Within the lung, the nanoparticles recruit immune cells so that the tumors don't take," explained Dr. Nicole Steinmetz, corresponding author of the study.
Demonstrating Dual Effects
In order to test the efficacy of the plant virus nanoparticles, the team conducted both prevention (prophylaxis) and treatment studies. For the prevention studies, the nanoparticles were injected into the bloodstreams of healthy mice. The animals were later injected with either melanoma or triple-negative breast cancer. Treated mice exhibited a considerable reduction of cancers spreading to the lungs in comparison to untreated mice.

For treatment studies, mice that had metastatic tumors in their lungs were administered the plant virus nanoparticles. These mice were found to show smaller lung tumors and longer survival than those that had not been treated.
Potential to Avert Re-emergence
What makes the findings of the study exceptionally important—according to the authors—is that the efficacy observed was against cancer cell lines that were extremely aggressive. "So any change in survival or lung metastasis is pretty striking. And the fact that we get the level of prevention that we do is really, really amazing," expressed Chung.
Dr. Steinmetz hopes that a treatment of this kind can benefit patients after they have undergone the removal of a cancerous tumor. "It wouldn't be meant as an injection that's given to everyone to prevent lung tumors. Rather, it would be given to patients who are at high risk of their tumors growing back as a metastatic disease, which often manifests in the lung. This would offer their lungs protection against cancer metastasis," she averred.
However, before the new treatment can reach the phase of application, it will have to undergo extensive evaluation. This includes pharmacology and immunotoxicity studies. The authors also added that future studies will focus on the exploration of combining the new treatment with other existing cancer therapies such as chemotherapy, radiation, or checkpoint drugs.

















