![[Representational image] Chronic Pancreatitis,health, gut,](https://data1.ibtimes.co.in/en/full/645113/chronic-pancreatitishealth-gut.jpg?h=450&l=50&t=40)
The gut is the gateway to heath, courtesy the teeming microbial minions. The smarter they are, the better you are.
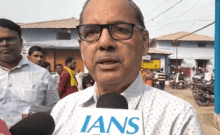
Indian scientists say tweaking the bacterial milieu in the intestine could be potentially therapeutic in treating chronic pancreatitis, a disease that cripples the body's ability to digest food and regulate blood sugar and could even lead to diabetes.
Their suggestion is based on the revelation that alteration in gut microbes may be linked to malnutrition and diabetes in chronic pancreatitis (CP) for which there is currently no definitive cure.
"Whatever treatment is offered to these patients is directed in ameliorating or reducing pain and improving nutritional and glycemic (blood sugar) status," Rupjyoti Talukdar, Clinicial Pancreatologist and Head of Pancreatic Research at Hyderabad's Asian Institute of Gastroenterology, told IANS.
Some of the futuristic procedures that could potentially contribute to therapy include administration of "designer" probiotics and faecal transplantation.
"Our recent studies have added a new angle to the disease biology of CP, i.e. alteration of the gut microbiota could contribute to diabetes and malnutrition. Gut microbial manipulation, including 'designer' probiotics and faecal transplantation, could be a potential future therapeutic addendum," Talukdar explained.
"However, before translating the concept to the clinic, this needs to be stringently tested in clinical trials," he cautioned.
It sounds incredible but the millions of microscopic bugs in our gut may have a major role to play in the progression of the disease.
Collective human gut micro flora is composed of a staggering 35,000 bacterial species.
A specific concoction of gut microbes is crucial for digestion of foods (such as breaking down complex carbohydrates), key to a normal immune system, fending off diseases and for producing many essential hormones and vitamins that the body cannot produce.
Whether the good ones triumph or the bad ones flourish, this good versus evil story unfolding in your belly determines your overall health.
In chronic pancreatitis, as the pancreatic tissue is damaged, digestive juices reduce and the undigested fat piles up, things start spiralling south for microbes.
"When there is excess amount of undigested fat in the intestine, there will be a change in the profile of healthy bacteria," Talukdar explained.
The study noted the reduction in numbers of two crucial bacterial species (F.Aprausnitzii and R. bromii) in individuals with CP. They are among the good bacteria needed to keep the tummy in top shape.
The gut flora is an entire ecological system by itself.
"Therefore by giving the entire intestinal flora in the form of faecal transplantation, the ecology will be maintained. This is important because the different groups of organisms in the intestine are interrelated in distribution and function," Talukdar said.
Faecal transplant is a real thing and has already found beneficial use in diseases of the intestine, namely, Clostridium difficile diarrhoea, which could result from antibiotic use or other conditions such as ulcerative colitis.
The other futuristic option, Talukdar said could be "personalised" probiotics that would act on specific targets and thereby provide the maximum possible therapeutic benefit to the patient.
Talukdar underscored the importance of dietary interventions, besides therapy.
"It can be done to a certain extent by ensuring adequate fat digestion with pancreatic enzyme supplementation, taking a balanced home-cooked diet without any specific restriction while on enzyme supplementation, and otherwise avoid high fat content in diet so as to prevent accumulation of inadequately digested fat in the intestinal lumen," he added.
The study, published in March in Nature's Scientific Reports, is co-authored by Sai Manasa Jandhyala, A. Madhulika, G. Deepika, G. Venkat Rao, D. Nageshwar Reddy, Chivukula Subramanyam and Mitnala Sasikala.