The SARS-CoV-2 coronavirus—especially some of its newer and lethal variants—is exceptionally adept in binding with human cells and infecting them. Therefore, therapies and treatments aimed at inhibiting the virus's binding with cells can serve as a game-changer in the fight against COVID-19. Now, scientists have developed 'nanodecoys' that can bind with the novel coronavirus and neutralize it.
According to the multi-institutional study, nanocells derived from human lung spheroid cells (LSCs), can not only bind with the SARS-CoV-2 virus but also block it and promote viral clearance. Using an animal model of COVID-19, the scientists demonstrated that the 'nanodecoys' mimicked the coronavirus' preferred receptor—the ACE2 (angiotensin-converting enzyme 2)—rather than attacking the pathogen itself. It was also found to reduce lung injury in the model.
"We have provided evidence in a non-human primate model of live SARS-CoV-2 infection that cell-derived and cell-mimicking nanodecoys can protect lung cells from the infection and damage caused by SARS-CoV-2," the authors wrote in the study that was published in the journal Nature Nanotechnology.
Hoodwinking the Virus
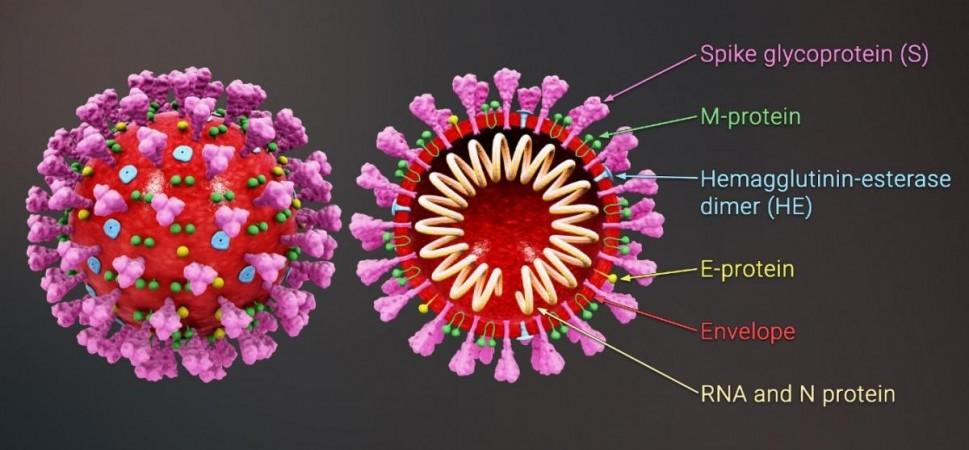
It has been well-established that the SARS-CoV-2 virus gains entry into human cells by predominantly targeting the ACE2 receptor, a protein found on the surface of several cell types. For this, it uses its 'spike' or 'S-protein'—a hook-like glycoprotein structure on its membrane—that binds with the ACE2 receptors of cells. Once it invades a cell, it infects it and turns it into a 'factory' producing its viral RNA proteins.
LSCs are a natural mixture of lung epithelial stem cells and mesenchymal cells (stem cells isolated from different sources which can metamorphose into other cell types). Interestingly, they also express ACE2. This feature led the authors to explore the potential of LSCs as vehicles to confound the novel coronavirus.
"If you think of the spike protein as a key and the cell's ACE2 receptor as a lock, then what we are doing with the nanodecoys is overwhelming the virus with fake locks so that it cannot find the ones that let it enter lung cells. The fake locks bind and trap the virus, preventing it from infecting cells and replicating, and the body's immune system takes care of the rest," said Dr. Ke Cheng, corresponding author of the study, in a statement.
Promoting Improved Viral Clearance
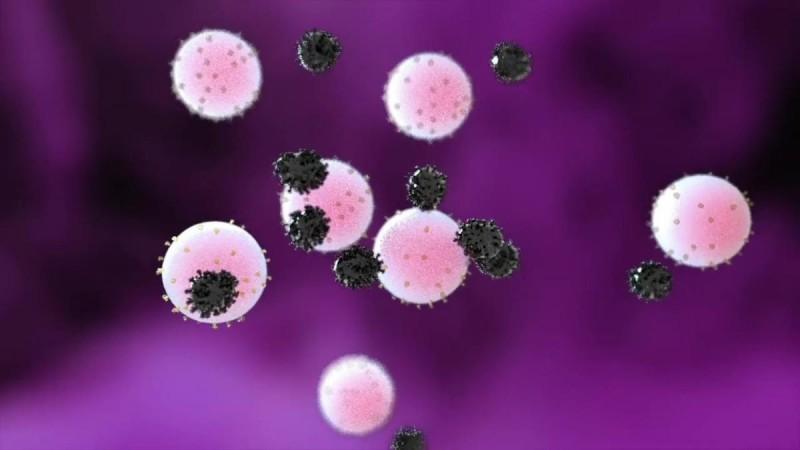
For the study, the researchers transformed individual LSCs into nanovesicles (i.e) minute cell membrane bubbles possessing ACE2 receptors and other proteins specific to lung cells on their surface. It was confirmed the 'spike' indeed bound with the ACE2 receptors present on the decoy cells in vitro. Next, they used an engineered SARS-Co-V-2 mimic virus for the purpose of in vivo testing in a mice model. The mice were administered the decoys intranasally through inhalation therapy. The nanodecoys were found to remain in the lungs of infected mice for 72 hours after the administration of just one dose and sped up the mimic virus' clearance.
Finally, to evaluate the veracity of these findings further, a pilot study was conducted in a macaque model. It was learnt that administration of the nanodecoys through inhalation therapy accelerated the clearance of the virus, and led to the reduction of fibrosis and inflammation in the lungs of the animals. No toxicity was observed either in the mice or macaque model.
However, the authors stated that additional studies are necessary to incorporate the therapy in human testing and to ascertain the exact mechanism of the nanodecoys' clearance from the body. "These nanodecoys are essentially cell 'ghosts,' and one LSC can generate around 11,000 of them. Deploying millions of these decoys exponentially increases the surface area of fake binding sites for trapping the virus, and their small size basically turns them into little bite-sized snacks for macrophages, so they are cleared very efficiently," explained Dr. Cheng.
Potential for Future Application
With several variants of the SARS-CoV-2 emerging at an aggressive rate, the nanodecoy therapy may possibly serve as a crucial treatment for COVID-19. Illustrating its potential, the authors enumerated three other benefits of the nanodecoys. Firstly, they can be delivered to the lungs non-invasively through inhalation therapy. Secondly, as the nanodecoys are acellular—consisting of nothing living within—they can be easily stored and can remain stable for longer periods; thereby facilitating their use off-the-shelf.
Lastly, LSCs have already seen application in other clinical experiments and trials. Therefore, they have increased prospects of use in the near future. "By focusing on the body's defenses rather than a virus that will keep mutating we have the potential to create a therapy that will be useful long-term. As long as the virus needs to enter the lung cell, we can keep tricking it," concluded Dr. Cheng.














