Beyond the conspiracy and bickering between the United States and China on who is responsible for the biowarfare, and healthcare workers at the frontline sparing no efforts to contain the spread of the virus, Africa, like many other continents, has announced a nationwide lockdown.
Economies are bleeding, mankind is feeling the unexpected pinch, globally advanced healthcare systems are questioned including the WHO and medical researchers, scientists are clocking in sleepless nights and long hours to find a vaccine at the earliest. No country across the globe at this point in time can pride itself on its immunity.
Two months after Egypt reported the first case of coronavirus in Africa, the pandemic seems to have affected the entire continent comprising 54 countries and 1.2 billion people. In fact, Lesotho which hadn't reported a case of the virus, also got its first COVID-19 positive diagnosis. With this, coronavirus has breached the entire continent.
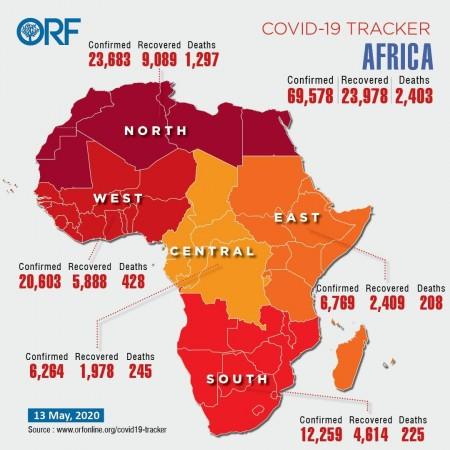
There are 69,578 coronavirus infections, 23,978 recoveries and 2,403 deaths in the region as of May 13, according to the Africa Centres for Disease Control and Prevention. Many African countries with fragile health-care systems are overwhelmed in the face of the COVID-19 outbreak. The countries worst affected by the pandemic in the African continent are South Africa with 10,652 cases, 9,746 cases in Egypt, 6,281 cases in Morocco and 5,891 cases in Algeria, according to the latest findings update from the John Hopkins University on May 12.
Covid-19 Impact on Africa: The Healthcare Dilemma
The virus has caught nations off guard, unprepared to deal with the crisis times in store. However, Africa wasn't among the first lot of countries to be affected by the pandemic, and the continent did get a month's window to prepare post warnings received from the WHO.
Most leaders neglected the threat and awakening call from WHO about the spread of Covid-19, and within a few weeks, densely populated Nigeria got infected with an alarming increase in COVID-19 cases to 151, spreading across the length and breadth of the nation to span 11 states and the federal capital territory. Years of absolute negligence and failure from the Nigerian government to fix the country's weak healthcare sector before the coronavirus outbreak in Africa brought to fore the health sham.
Besides weak healthcare infrastructure, a severe shortage of PPE kits and specialized equipment such as ventilators is a growing concern. The Sub-Saharan African countries are anyways battling some of the world's serious underlying conditions of Tuberculosis, HIV, and malnutrition to compromise on the health of millions of children born in the region, and other comorbidities.
If this wasn't enough, the humanitarian crisis as a result of the Boko Haram conflict in the northeast region of Africa has internally displaced more than 1.8 million people, to leave more than 7-million in need of urgent life-saving assistance that includes food, water and healthcare. These people, the victims of insurgency are at a higher risk of being contracted with COVID-19 and it is required of the government now to take immediate steps to cushion the effect of a raging pandemic in IDP camps and more needs to be done.
Most South Africans live on a hand-to-mouth existence working in informal jobs with no income security and hence have no health insurance. Most of the South Africans unemployed are reliant on the free healthcare system (already swamped) and social grants provided by the government for living expenses. With no access to medical aid in case of flu-like symptoms, the lower segments of society are reliant on home remedies, and if the condition gets worse they rush to small clinics nearby that are overly crowded to get access to basic generic drugs such as paracetamol and cough syrup.
According to ORF Online Covid-19 tracker, the Covid-19 cases in Africa region-wise are: North Africa records the highest with 23,683 cases, West Africa - 20,603 cases, South Africa - 12,259 cases, Central Africa - 6,264 cases and East Africa - 6,769 cases recording the total tally at 69,578 cases in the African continent as of May 13, 2020.
Lack of healthcare infrastructure and frontline medical professionals
With a surge in COVID-19 cases, a Reuters survey highlighted that there are less than one intensive care bed and one ventilator per 100,000 people in Africa. According to researchers, even in the best-case scenario, the African continent will need at least 10 times the current number of intensive care beds and ventilators as the outbreak peaks.
A poll 54 countries conducted by Reuters and responses received from health officials or independent experts in 48 of them reveal a shortage of national health systems. Also, low-levels of testing gears and equipment make it increasingly difficult to detect the exact number of COVID-19 cases in the region.

The United Nations Economic Commission for Africa (UNECA) has said, "Africa could see nearly 123 million cases this year, causing 300,000 deaths."
Africa's testing capacity is increasing steadily but it has conducted only around 685 tests per million people, according to Reuters' tally of figures from the Africa Centres for Disease Control and Prevention (Africa CDC).
While many African governments moved quickly to contain the pandemic, restricting movement, mounting high-profile public health campaigns and repurposing factories to produce protective equipment, the pace was still slow.
Reuters survey states, "Africa could need at least 111,000 more intensive care beds and ventilators. WHO (World Health Organisation) publicly criticized the East African nation of Tanzania for not restricting large gatherings - it has gone for days without updating the current coronavirus figures and has further refused to divulge any details about its public health resources to donors."
As regards to testing conducted in Africa, the Reuters survey stated, "South Africa accounts for 30% of Africa's tests, although it has less than 5% of the population. Nigeria, which has 15% of the population, has carried out just 2% of testing; it began by testing strategically then broadened it out," Health Minister Osagie Ehanire said. Chad and Burundi have carried out fewer than 500 tests each. Chad didn't have enough testing kits and neither staff as many of them had fallen ill; Burundi did not respond. Tanzania carried out 652 tests and identified 480 cases."

Further shortage of healthcare workers is a pressing concern in the region. According to a World Economic Forum report, Africa cannot afford to lose its healthcare workers. It states, "Zambia's healthcare system is already overburdened, with one doctor for every 10,000 people. Before COVID-19, statistics show that over 40% of WHO Member States have less than 10 medical doctors per 10,000 population; 26% have less than 3. Healthcare workers are distributed unevenly across the globe. Countries with the lowest relative need have the highest numbers of healthcare workers, while those with the greatest burden of disease must make do with a much smaller healthcare workforce. Africa suffers more than 22% of the global burden of disease but has access to only 3% of healthcare workers, and less than 1% of the world's financial resources."
Donation Diplomacy from China
China did express its intent to help Africa cope with the COVID-19 crisis armed with economic muscle and soon embarked on donation diplomacy - distribution of PPEs, medical gears and supplies to African countries. The initial beneficiaries of the donation were Ethiopia, Algeria, Nigeria, South Africa, Zimbabwe, Cameroon and other countries.
Jack Ma, billionaire and co-founder of Alibaba Foundation donated testing kits, a string of medical masks, protective face shields and protective clothing. The consignment of such medical donations was transported by Ethiopian Airlines. China in its efforts is looking at a win-win partnership with Africa.
While West Africa continues to dwell in a state of confusion with increasing fatalities and number of cases, the new paradigm shift brought about by COVID-19 outbreak has taught global economies and healthcare systems to be increasingly self-reliant in terms of research, human resource, skilled knowledgeable professionals and vaccine production, instead of being import-dependent on other nations.














