Burn wounds are among the most trickiest and serious one to treat. Not only do they cause immeasurable pain but can result in damage that can lead to significant tissues loss or even death. Thus, timely and effective treatment is key in mitigating further harm. Now, scientists have demonstrated that light therapy may accelerate the healing of burns.
According to a new study, photobiomodulation—a form of light therapy—was found to expedite the recovery from burns and reduce inflammation in a mice model. It did so by activating a protein known as TGF-beta 1/ TGF-β1 which is associated with cell division and growth. The study was published in the journal Nature Scientific Reports.
"These results suggest activation of endogenous latent TGF-β1 following PBM treatments plays a key role in burn wound healing. These mechanistic insights can improve the safety and efficacy of clinical translation of PBM treatments for tissue healing and regeneration," the authors wrote.
Light Therapy and Healing

The damage caused by burn injuries is not confined to just cosmetic defacement. According to the WHO, approximately 180,000 deaths occur across the world every year. These injuries also expose victims to other morbidities such as secondary infections by opportunistic pathogens that can prove fatal. On a social level, the scarring—depending on the degree of burn—can cause distress and invite stigmatization.
Photobiomodulation (PBM) therapy uses non-ionizing forms of light sources. This includes sources such as broadband light, LEDs, and LASERS, falling within the near-infrared and visible spectrum. "Photobiomodulation therapy has been effectively used in supportive cancer care, age-related macular degeneration and Alzheimer's disease. A common feature among these ailments is the central role of inflammation," explained Dr. Praveen Arany, lead author of the study in a statement.
Numerous academic papers and clinical trials have demonstrated the efficacy of managing pain and promoting healing. Therefore, the scientists wanted to ascertain what role PBM could play in the healing of burn wounds.
Triggering a Crucial Protein
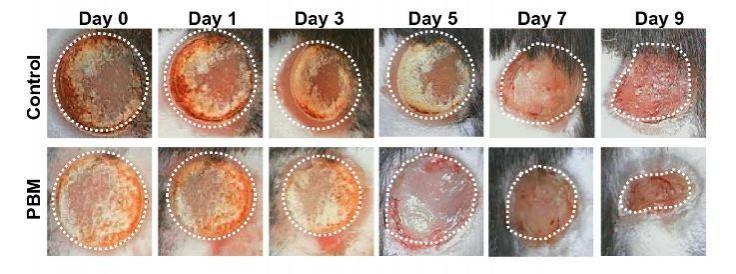
For the study, the authors employed a modified burn wound model. Using an in vitro model, they first established the safe and effective levels of laser exposure that could promote healing without potentially exacerbating the wound. This helped them optimize a protocol for the PBM treatment. Following this, they examined the effect of PBM on the closure of third-degree burns in mice over the course of nine days. In comparison to control animals, burn wounds treated with PBM showed considerably improved healing.
So what led to the superior repairing of burn wounds by PBM treatment? The team found that the therapy triggered TGF-beta 1. It is a protein that performs several cellular functions. This includes cell differentiation, controlling of cell growth and division, and apoptosis (programmed cell death).

TGF-beta 1 in turn, stimulated several cell types closely associated with tissue repairs such as fibroblasts and macrophages. Fibroblasts are the most common type of connective tissue cells in the body that help maintain the structural integrity of several tissues. Macrophages are cells of the innate immune system that detect, ingest (phagocytosis), and eliminate cell debris and pathogens.
"This work provides evidence for the ability of photobiomodulation-activated TGF-beta 1 in mitigating the inflammation, while promoting tissue regeneration utilizing an elegant, transgenic burn wound model," said Dr. Arany.









!['Had denied Housefull franchise as they wanted me to wear a bikini': Tia Bajpai on turning down bold scripts [Exclusive]](https://data1.ibtimes.co.in/en/full/806605/had-denied-housefull-franchise-they-wanted-me-wear-bikini-tia-bajpai-turning-down-bold.png?w=220&h=138)



