Vaccination is the most important weapon in the fight against COVID-19. However, several variants of the SARS-CoV-2 virus—with mutations that help them evade vaccine-enabled immunity—have appeared over the past few months. This has raised worries about the protection offered by existing vaccines against mutants. Providing some good news in this regard, scientists have found that naturally occurring immune cells can target a key protein in the coronavirus.
Through a new study, researchers from the University of California, Los Angeles, have discovered that certain receptors found on T cells (a type of lymphocyte) can recognize a protein known as viral polymerase in the SARS-CoV-2 virus.
They also gleaned that receptors that identified the SARS-CoV-2's viral polymerase helped T cells mount an immune response not just against the virus but also other coronaviruses such as MERS (Middle East respiratory syndrome) and SARS (Severe acute respiratory syndrome).

The findings were published in the journal Cell Reports. "Current vaccines provide significant protection against severe disease, but as new, potentially more contagious variants emerge, researchers recognize that vaccines may need to be updated — and the new UCLA findings point toward a strategy that may help increase protection and long-term immunity," the university said in a statement.
Rethinking Vaccination Approach
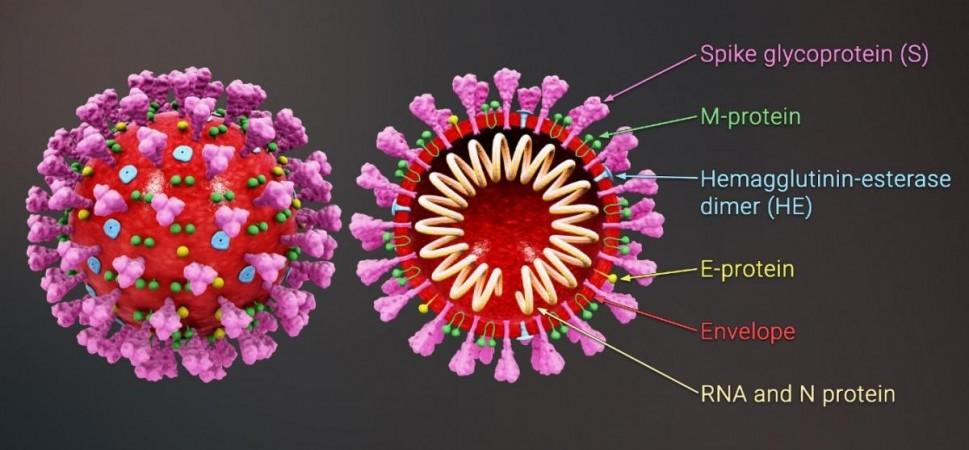
Nearly all approved COVID-19 vaccines utilize a section of the spike protein—a hook-like structure that the SARS-CoV-2 virus uses to invade cells—to elicit an immune response against the pathogen through the production of antibodies. Unfortunately, multiple newer variants of concern (VOC) such as Delta and Omicron, whose spike proteins carry numerous mutations that enable immunoevasion, have emerged.
These spike-borne mutations make it difficult for antibodies and immune cells (triggered by vaccination) to identify the variants. Thus, vaccines that have a more extensive and robust immune response are the need of the hour. One way of accomplishing this goal is the inclusion of varied viral proteins in vaccines. Proteins that are less susceptible to mutations and can initialize T cells may serve as ideal candidates for this.
T cells are lymphocytes forming an integral part of the body's adaptive immune system. Their surfaces contain receptors that recognize antigens (i.e) foreign protein fragments. When T cells come in contact with an antigen that their receptors recognize, they undergo self-replication and produce more immune cells. Some of these T cells instantly target and destroy infected cells, while others circulate within the body to combat the same infection in the event of its re-emergence.
Targetting a Key Protein
The current study was centered on viral polymerase protein, a nucleic acid that plays a crucial role in the replication and transcription of the viral genome. It is not exclusive to the SARS-CoV-2 virus and is found in other pathogenic viruses such as the common cold, MERS (Middle East respiratory syndrome), and SARS (Severe acute respiratory syndrome), among many others.
Viral polymerases function as engines employed by coronaviruses to make copies of themselves, thereby, aiding in the spread of infection. While the spike protein undergoes numerous mutations as the virus evolves, the likeliness of viral polymerases mutating or changing is remote.
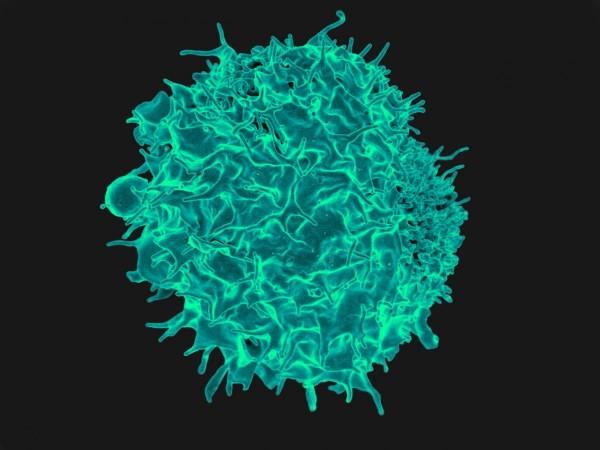
In order to ascertain whether the human immune system possesses T cell receptors (TCRs) that can recognize viral polymerase, the team exposed blood samples—obtained before the COVID-19 pandemic—from healthy individuals to the SARS-CoV-2 viral polymerase antigens [RNA-dependent RNA polymerase (RdRp/NSP12)]. Interestingly, it was observed that certain T cell receptors were able to recognize the polymerase.
Recognition By Immune Cells
Next, the researchers turned to a technique called CLInt-Seq to sequence the receptors genetically. Following this, T cells were engineered to bear these receptors that targeted the viral polymerase. This enabled the researchers in studying the receptors' capacity to recognize and neutralize the SARS-CoV-2 virus and other disease-causing coronaviruses.
The scientists found that two RdRp epitopes (part of an antigen recognized by immune cells) were able to activate broadly coronavirus reactive T cell responses. Cytotoxic analysis revealed that most of the TCRs recognized and killed RdRp expressing cells. Additionally, the TL9 (an epitope) reactive TCR exhibited strong cross-reactivity with SARS, MERS, 229E, and NL63 coronaviruses.
However, the authors admitted that the study was bound by a few limitations. "We show that RdRp specific TCRs recognize processed epitopes in a reconstructed system of viral infection, however, we do not show direct control of live SARS-CoV-2 virus," they wrote. They also added that the study did not show an association between T cell responses that were identified and disease severity.
Nevertheless, the findings have the potential to inform the future development of COVID-19 vaccines. It could help in the devising of a strategy that may aid in the maximization of protection and long-term immunity. "This study provides a strong basis for considering the development of vaccines against either specific epitopes or the full-length RdRp," wrote the authors.

















