COVID-19 pandemic has taken a heavy toll on everyone's lives, especially those who have had to deal with the virus, either by watching their loved ones suffer in agony or have to go through the experience themselves. More than the physical strain, COVID-19 has left a scar on mental well-being. When COVID-19 strikes, or even when one starts to show early symptoms of the infection, panic takes over and we're left with endless thoughts of what's going to happen next. It gets more challenging when a situation like the one in India arises, where hospitals are overwhelmed with COVID patients and there's an acute shortage of oxygen, ventilators and drugs needed to fight the virus. You're left with nothing but to act on your own but without panic.
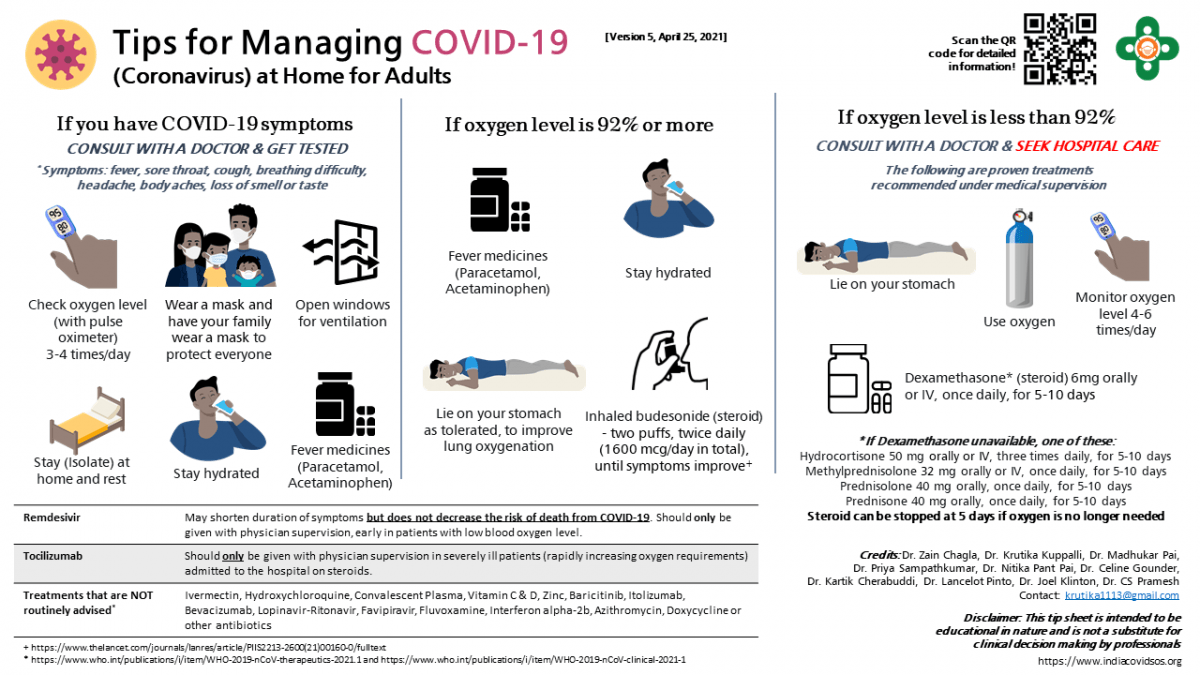
Firstly, one needs to understand the symptoms of COVID-19, the early, the better. Symptoms of COVID-19 include fever, sore throat, dry cough, headache, body aches, and loss of smell or taste. Here's what you need to do in case you have these symptoms. These guidelines are sourced from India COVID SOS, a website that is designed to help people deal with early signs of COVID-19. In case of severe symptoms, a doctor's intervention is recommended.
Trying to get tested using the RT-PCR method is a priority, but one mustn't sit idle waiting for the test results. If you have one or more symptoms and likely exposed to the virus, chances are you have the infection and it's best to start taking the precautions.
Regardless of your COVID-19 test result, follow these steps below.
First line of defense
Stay at home, preferably in isolation and away from other family members.
Wear a mask that perfectly covers mouth and nose and advise everyone in your house to wear one as well.

Keep windows in the house open for better ventilation.
Drink lots of water and fluids with salt and sugar.
Take paracetamol to reduce fever, headache and body pain. You can take up to 4 times a day, one tablet each.
Check your SpO2 levels 3-4 times a day using a pulse oximeter, which can be purchased from any pharmacy.
COVID-19 positive with oxygen saturation levels 92% or higher
First and foremost, one needn't panic. You need not go to the hospital right now.
Monitor your SpO2 levels 3-4 times day, make a chart if possible. Increase monitoring if you've breathing difficulty.
Drink lots of fluids as recommended above.
Lie on your stomach in prone position or on side, especially if you've difficulty breathing. This improves oxygen levels.

Continue taking Paracetamol, but do not start taking steroid pills at this stage. Not even Remdesivir and Tocilizumab at this stage.
A chest X-ray or CT scan is also not needed at this point.
Use steroid inhalers (budesonide) if you are over 50 years. Use two puffs of steroid inhaler (budesonide) twice a day for 5-7 days if you have it available; if the puff inhaler version is unavailable, you can also buy dry powder inhalers.
COVID-19 positive with oxygen saturation levels below 92%
It's time to consult a doctor and based on their recommendation, get admitted to a hospital. According to India COVID SOS, a website that is designed to help COVID patients based on recommendations from health experts, the use of these steps below under medical supervision can be helpful:
Use the minimum amount of oxygen needed to keep your oxygen saturation above 92%.
Take a steroid medication. Any of the options listed below can be used (after doctor's consultation). Oral forms are preferred if you are at home, intravenous forms may be used in the hospital
- Dexamethasone 6 mg once a day
- Methylprednisolone 32 mg once a day
- Prednisolone or Prednisone 40 mg once a day
- Hydrocortisone 50 mg three times a day
Steroids are usually given for 5 – 10 days and can be stopped once oxygen is no longer needed. There is no need to taper them down.
If you have diabetes, monitor your blood sugar while on steroids and if they are higher than normal make sure to let your doctor know
Lie flat on your stomach or on your side alternating with lying on your back to help improve oxygen levels.
Stay in touch with a doctor and seek help if your oxygen needs increase to more than 4L/minute.
For severely ill patients, hospitals might use drugs such as Remdesivir or Tocilizumab (these are strictly not to be used at home and not to be used without expert supervision).
Medicines not proven for COVID treatment
- Azithromycin
- Baricitinib
- Bevacizumab
- Convalescent Plasma
- Doxycycline
- Favipiravir
- Fluvoxamine
- Hydroxychloroquine
- Itolizumab
- Interferon alpha-2b
- Ivermectin
- Lopinavir-Ritonavir
- Vitamin C
- Vitamin D
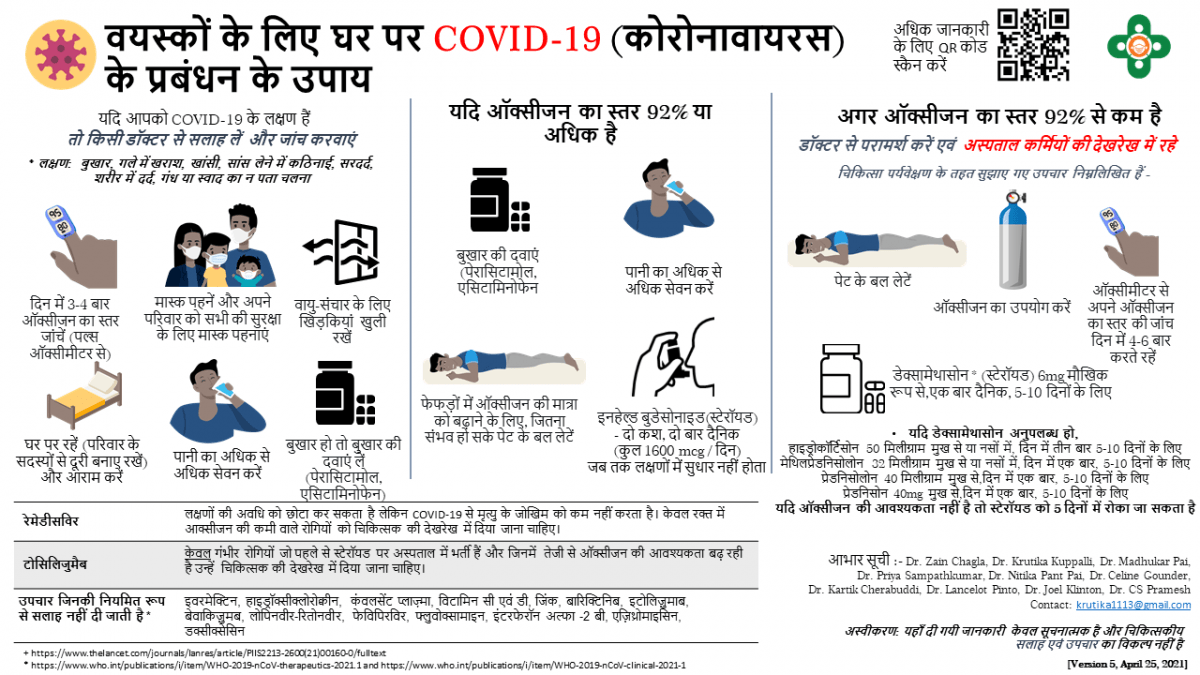
Check out these infographics for easier reference:
These guidelines are NOT INTENDED TO BE A SUBSTITUTE FOR INDEPENDENT PROFESSIONAL LEGAL ADVICE, MEDICAL JUDGMENT, DIAGNOSIS, OR TREATMENT.

















