A medication used to treat HIV can prevent spreading of prostate cancer to the bones, researchers reveal.
Experiments conducted on mice showed that maraviroc, a CCR5 (chemokine receptor type 5) receptor antagonist used in HIV therapy was highly effective against prostate cancer metastasis.
CCR5 receptor is a protein found on the surface of white blood cells in the immune system, which has been known to play a huge role in AIDS and metastatic breast cancer.
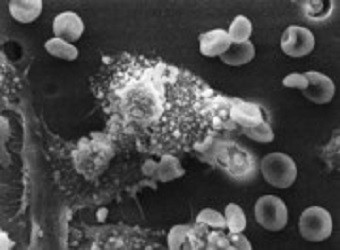
Metastasis is a term used to describe spread of a deadly cancer from its original site to other parts of the body -- mainly to bones, lungs and liver.
In prostate cancer, metastasis strikes bones and lymph nodes than other parts of the body. Lymph nodes are the bean-shaped glands and are part of the immune system that transports nutrients, fluids and waste material between tissues and bloodstream. The condition, according to experts at the Mayo Clinic, occurs when the cells break away from the tumour to the lymphatic system, which carries it to the other parts of the body.
A 2012 study carried out by Dr Richard Pestell and colleagues from the Thomas Jefferson University in US had shown that CCR5 receptor played a major role in spreading of breast cancer to the lungs.
In the new study, researchers found that maraviroc lowered the risk of metastasis in mice with prostate cancer. The overall metastatic load in bone, brain and other organs dropped by 60% after the rodents took maraviroc.
To confirm the role of CCR5 in metastasis, researchers analysed genomic data of prostate cancer patients. Results showed that CCR5 was highly expressed in prostate cancer and metastases than normal tissue sand primary tumours. Researchers also found that higher expression of the CCR5 genes shortened length of survival.
"In fact, we noticed that patients who had a lower expression of the CCR5-pathway genes had a longer survival times, whereas high expression of these CCR5 genes was associated with a shorter overall survival," co-first author of the study Dr Xuanmao Jiao, an instructor in the department of Cancer Biology at Jefferson, said in a news release.
The study has been published in Cancer Research.









