Since the onset of the COVID-19 pandemic, the ultimate goal of doctors across the world has been to prevent the death of patients infected with the SARS-CoV-2 coronavirus. Several factors have been attributed to the prognosis of the infection. One such factor is the use of medications for pre-existing conditions. Now, scientists report that the use of statins, commonly prescribed drugs for lowering blood cholesterol, may help reduce the risk of in-hospital death in COVID-19 patients.
According to the new study, in COVID-19 patients who used statin medications prior to their hospitalization, a 41 percent lower risk of death due to the viral infection was observed. Over 25 percent in the reduction of severe outcomes was also noted. The findings of the study—which builds on previous research—were published in the journal PLOS ONE.
"Patients taking statins prior to hospitalization for COVID-19 had substantially lower odds of death, primarily among individuals with a history of CVD and/or hypertension. These observations support the continuation and aggressive initiation of statin and anti-hypertensive therapies among patients at risk for COVID-19, if these treatments are indicated based upon underlying medical conditions," wrote the authors.
Lowering Cholesterol and Keeping COVID-19 Away?
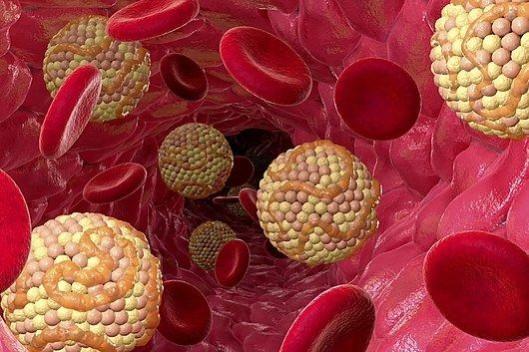
It has become common knowledge that the SARS-CoV-2 uses the ACE2 (angiotensin-converting enzyme2) receptor—an enzyme found on several cell types—to invade cells. Interestingly, ACE2 serves as the regulatory target of statins.
"When faced with this virus at the beginning of the pandemic, there was a lot of speculation surrounding certain medications that affect the body's ACE2 receptor, including statins, and whether they may influence COVID-19 risk," said Dr. Lori Daniels, lead author of the study, in a statement.
Therefore, Dr. Daniels and her colleagues, hypothesized that statins may impede COVID-19 infection via their noted binding capabilities and anti-inflammatory effects. She posited that this may probably prevent the progression of the disease. Statins are commonly prescribed to patients with high blood cholesterol levels in order to reduce it. It works by blocking enzymes in the liver that are responsible for the production of cholesterol.
The current study develops on an older one led by Dr. Daniels, which sought to test her conjectures. 170 anonymized medical records of patients who were being treated at UC San Diego Health for COVID-19 were examined. It was found that the use of statin prior to hospitalization for the viral infection led to an over 50 percent decrease in the risk of developing severe disease. Therefore, the team aimed to apply these findings to a larger group of participants.
Investigating A Larger Cohort

For the study, the authors utilized data from American Heart Association's COVID-19 Cardiovascular Disease Registry. The anonymized medical records of 10,541 patients (mean age was 66 ± 14 years) were examined by the team. These patients had been admitted for COVID-19 care over the course of nine months—from January 2020 to September 2020—across 104 hospitals in the US.
Before hospitalization, 42 percent of the subjects were using statins (n = 4,449; 7 percent on statin alone, 35 percent on statins along with anti-hypertensives). Other aspects taken into consideration included pre-existing conditions and comorbidities such as hypertension, cardiovascular disease (CVD), and diabetes, among others.
Using statistical matching methods, the researchers compared outcomes for patients taking statins or anti-hypertension medication to those in patients of similar condition who were not on such medication. "We matched each patient to one or more similar patients, using hospital site, month of admission, age, race, ethnicity, gender, and a list of pre-existing conditions, in order to make the two groups as comparable as possible" explained Dr. Karen Messer, co-author of the study.
Marked Reduction in Risk of Death

Within the analyzed population, 2,212 (21 percent) died (or were discharged to hospice care) and 4,161 (39 percent) had severe outcomes. The propensity-score matched analysis in participants with no history of hypertension/CVD revealed that the use of medication was associated with an 8 percent decrease in the chances of severe outcomes. A similar analysis in subjects with a history of hypertension/CVD showed that the use of these drugs resulted in 20 percent reduced odds of a severe outcome and 30 percent lower chances of death.
In totality, statin use before hospitalization was associated with a decrease in mortality by 41 percent. A reduction of over 25 percent in the risk of developing severe outcomes was associated with the use of statins. The magnitude reduction in this risk was greater than what was seen for the use of anti-hypertension drugs alone.
According to Dr. Daniels, it is patients with just medical causes such as high blood pressure or CVD who seem to have benefitted the most. The team stated that in COVID-19 patients with CVD or high blood pressure, the use of stains or high blood pressure was linked to a 32 percent lower risk of death.
Admitting to the limitations of the study, Dr. Daniels averred: "As with any observational study, we cannot say for certain that the associations we describe between statin use and reduced severity of COVID-19 infection are definitely due to the statins themselves; however, we can now say with very strong evidence that they may play a role in substantially lowering a patient's risk of death from COVID-19."









!['Had denied Housefull franchise as they wanted me to wear a bikini': Tia Bajpai on turning down bold scripts [Exclusive]](https://data1.ibtimes.co.in/en/full/806605/had-denied-housefull-franchise-they-wanted-me-wear-bikini-tia-bajpai-turning-down-bold.png?w=220&h=138)



