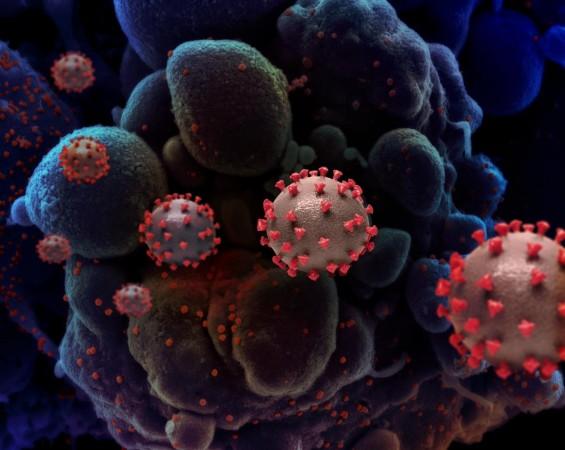
The onslaught of the SARS-CoV-2 virus is accompanied by several complications. These include increased inflammation of blood vessels and the formation of abnormal clots within them, particularly in the lungs. This is said to worsen the prognosis of COVID-19 patients. Now, a new study suggests that the early administration of a standard blood-thinning drug in moderately ill hospitalized patients may stop the process of thrombo-inflammation and decrease the risk of acute disease and death.
According to the study by an international team of researchers, a full dose of Heparin—a blood thinner—administered to moderately ill COVID-19 patients early on, can decrease the odds of death. The preprint of the study—which also looked at data from other large trials— was made available on the platform MedRxiv.
"We believe that the findings of our trial and the multiplatform trial taken together should result in a change in clinical practice for moderately ill ward patients with COVID-19," said Dr. Michelle Sholzberg, first author and co-principal investigator of the study, in a statement.
Helping Mitigate Clots
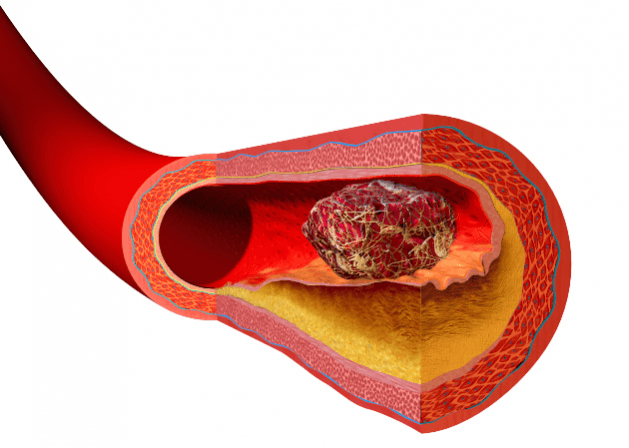
Heparin is an anticoagulant—it thins the blood and prevents the formation of clots. It is used to treat people who have medical conditions such as venous thrombosis (blood clots in veins) and pulmonary embolism (blood clots that have traveled to the lungs). Heparin is also used in individuals who are undergoing medical procedures such as arterial angiography that increase the risk of clot formation. In addition to its anticoagulation properties, it is also known for its anti-inflammatory effects.
The study, an open-label randomized international multi-center clinical RAPID Trial—which is also known as the RAPID COVID COAG – RAPID Trial—investigated what benefits the administration of heparin offered. The authors compared the action of a therapeutic full dose of the drug with that of a prophylactic low dose in hospitalized COVID-19 patients with moderate cases of the viral infection.
Reduced Risk of Death

Explaining the primary outcome of the trial, a composite of multiple factors, Dr. Mary Cushman, co-principal investigator, said, "This study was designed to detect a difference in the primary outcome that included ICU transfer, mechanical ventilation or death." Hospitalized patients with moderate COVID-19 and elevated D-dimer levels (a measure of clots)were randomly assigned to prophylactic or therapeutic heparin groups.
In 37 of the 228 patients (16.2 percent), who had received therapeutic full dose heparin, the primary outcome was witnesses at day 28. A low dose of heparin in the prophylactic group was found to help 52 of 237 (21.9 percent) reach primary outcome during the same duration as the other group. Four patients (1.8 percent) receiving therapeutic heparin succumbed to the infection while 18 patients (7.6 percent) who were administered prophylactic heparin died of the viral infection.
"While we found that therapeutic heparin didn't statistically significantly lower incidence of the primary composite of death, mechanical ventilation or ICU admission compared with low dose heparin, the odds of all-cause death were significantly reduced by 78 percent with therapeutic heparin," stated Dr. Sholzberg.
Strong Evidence of Benefits
Dr. Peter Jüni, co-principal investigator of the study, noted that the team also submitted a meta-analysis of randomized evidence comprised of data from other large trials. This included ATTACC (Antithrombotic Therapy to Ameliorate Complications of COVID-19), ACTIV-4a (Anti-thrombotics for Adults Hospitalized With COVID-19 A), and REMAP-CAP (Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia). The data suggested that therapeutic heparin may indeed benefit hospitalized patients with moderate COVID-19.
He also added that another meta-analysis in the preprint of the study evidenced that while therapeutic heparin benefits hospitalized COVID-19 patients with moderate illness, it did not do so in severely ill patients admitted to the ICU. Talking about the RAPID trial, Dr. Cushman expressed: "We called this trial 'The Little Engine that Could,' because of the sheer will of investigators around the world to conduct it."