The loss of sight is one of the most crippling obstacles that can severely curtail one's quality of life. In several cases, the loss is irreversible. Offering hope, a new study has reported the first successful clinical application of optogenetics to restore the vision of a 58-year-old man suffering from a degenerative retinal disease for 40 years.
According to the study, researchers used optogenetics—a biological technique involving the combination of optics and genetics—to partially restore the vision of a man suffering from Retinitis pigmentosa (RP). The study involved the injection of light-sensitive proteins into the participant's retina directly, which eventually enabled him to distinguish images using specialized goggles.
"This is the first reported case of partial functional recovery in a neurodegenerative disease after optogenetic therapy," wrote the authors in the study, that was published in the journal Nature Medicine.
Skipping Damaged Cells
Retinitis pigmentosa refers to a group of rare, genetic disorders that involve malfunctioning and loss of cells in the retina—the light-sensitive tissue found at the back of the eye. RP destroys the photoreceptor cells in the eye, thereby, impeding the very first step in the visual pathway. In individuals with healthy retinas, light is detected by photoreceptors which transmit signals to retinal ganglion cells (RGCs), which ultimately relay the signal to the brain.
Optogenetics is a technique where flashes of light are used to control gene expression and neuron firing. It is used widely to investigate neural circuitry, and is being looked into for the potential treatment of brain disorders, pain, and blindness.
GenSight Biologics, the Paris-based company conducting the trial, recruits individuals with RP. It employs an optogenetic therapy that entirely skips the involvement of damaged photoreceptors. Here, a virus is used to carry light-sensitive bacterial proteins to the RGCs directly and helps them detect images firsthand.
Helping Create An Image
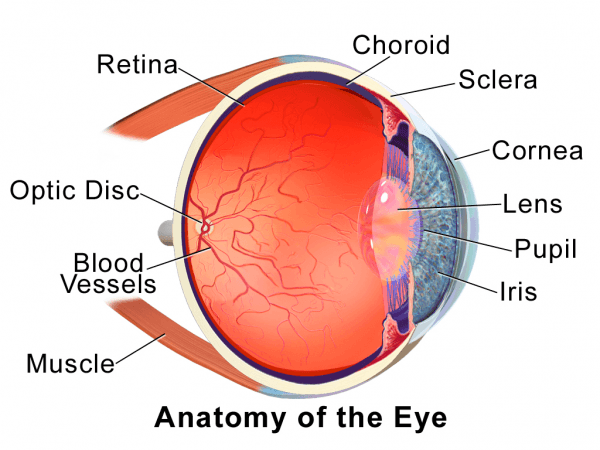
For the study, a man who had been diagnosed with RP 40 years ago, was injected with the virus. This was followed by a four-month wait for the stabilization of protein production by RGCs before his vision could be tested. A healthy human retina utilizes several light-sensitive proteins and cells to see a wide range of light. Therefore, one of the challenges of the study was regulating the quantity of and the kind of light entering the eye of the RP patient.
"No protein can replicate what the system can do," said Dr. José-Alain Sahel, lead author of the study, in a statement. In order to overcome this hurdle, the authors designed a set of goggles that could capture visual information in the surroundings of the man and enhanced it for easy detection by the bacterial proteins in the RGCs.
The goggles uses a camera to examine the changes in brightness and contrast. It converts the changes in real-time into amber-colored dots which Dr. Sahel says resembles a 'starry sky'. The proteins in RGCs are activated when the light from these dots enters a person's eyes. This leads to the RGCs relaying a signal to the brain, where the patterns are ultimately resolved into an image.
Sight At Last

Being able to 'see', however, required some training. The participant trained for several months with goggles while his brain adjusted and began accurately interpreting the dots. "He was like an experimentalist, a scientist trying to understand what he was seeing and make sense of it," expressed Dr. Sahel.
Over time, the participant was able to discern high-contrast images such as white stripes in a crosswalk or objects on a table. Interestingly, the analysis of his brain activity revealed that the visual cortex was responding to the image like how it would if he possessed normal sight.
Though the man still cannot see without the use of the goggles, Dr. Sahel said that he continues to wear them for several hours a day. His vision is also said to have improved since receiving the injection two years prior. Six other participants had received the light-sensitive protein injections last year. However, the COVID-19 pandemic prevented their training using the goggles. The team hopes to obtain results within a year or so.
Safe With Future Scope

The revolutionary technique has received some positive welcome. John Flannery, a neurobiologist at the University of California, Berkeley, remarked: "It's a big step for the field. The most important thing is that it seems to be safe and permanent, which is really encouraging."
It is a fact that a healthy retina contains over 100 times the photoreceptors than RGCs do. Therefore, the resolution of the images detected by the RGCs may never be able to replicate natural vision. Flannery, nevertheless, quipped that the ability of the brain to interpret these images correctly was exciting.
Sheila Nirenberg, a neuroscientist at Weill Cornell Medical College, opined that further research into the area was necessary. "It's interesting, but it's an N of 1," she noted. Nirenberg also said that she is looking forward to seeing whether others in the trial, including those who received higher doses of the protein injection, presented similar results.














